Abstract
Mortality following HSCT in pts with SAA over the age of 40 is reported to be in the order of 50%; international guidelines recommend first line immunosuppressive therapy above the age of 40. The aim of this study is to assess whether this is still true in 2015.
We used the Working Party for SAA (WPSAA) of the European Blood and Bone Marrow Transplantation Registry (EBMT), and identified 768 patients, aged 40 years or more, with acquired SAA , who underwent an allogeneic HSCT between 2001 and 2015.. Pts were divided in two transplant eras: 2001-2009 (n=329) and 2010-2015 (n=439). In the 2010-2015 period pts were older (52 vs 50 years, p<0.01), were more often grafted from alternative donors (ALT) (52% vs 28%, p<0.01), with a greater use of BM (53% vs 42%, p<0.01), and more often received a fludarabine containing regimen (60% vs 42%, p<0.01), and ATG or Campath (87% vs 67%, p<0.001).
The 5 year OS of patients grafted in 2001-2009 was 61% , compared with 58% for pts grafted in 2010-2015 (p= 0.9). In multivariate analysis including the interval between diagnosis and transplant, the patient's age, donor type, stem cell source , the use of fludarabine and ATG or Campath, the lack of improved survival in 2010-2015 was confirmed (RR 0.9, 95%CI 0.7-1.19; p=0.5). A very strong age effect was shown both in univariate and multivariate analysis: 5 year OS of patients aged 40-49 years, 50-59 years and >60 years , was respectively 66%, 57%, 40% (p<0.0001). The second favorable predictive factor was the use of either ATG or Campath (RR 0,58- 95%CI 0.43-0.76, p=0.002)
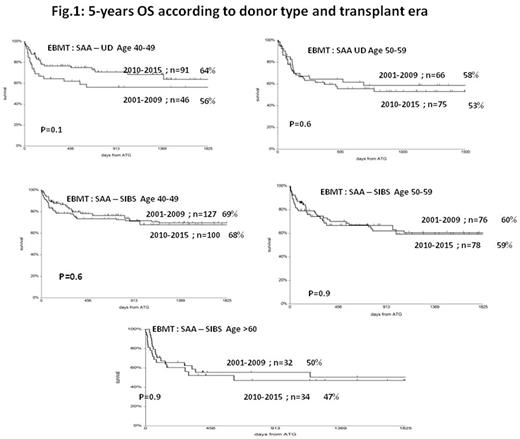
Regarding HSCT from HLA identical siblings, we could show identical 5 year survival for pts aged 40-49 years in 2010-2015 as compared to 2001-2009 (67% vs 70% p=0.8); for patients aged 50-59 years (59% vs 60%, p=0.9) and patients over 60 (47% vs 50%, p=0.9). For UD the 5 year survival in pts aged 40-49 was 64% in 2010-2015, vs 56% in the earlier period (p=0.1), and 53% vs 58% (p=0.6) for pts aged 50-59. The numbers were too small for comparison in patients over 60, with only 8 patients grafted in the 2001-2009 period; 61 patients were grafted in 2010-2015 with a 47% actuarial 5 year survival. (Figure 1).
Combined primary and secondary graft failure was reduced from 16% to 12% in the two time periods (p=0.02), acute GvHD grade II-IV was reduced from 15% to 11% (p=0.1) and chronic GvHD was also reduced from 31% to 25% (p=0.01). Infections remain the leading cause of death in both transplant eras (18% and 22% respectively), followed by GvHD (5% and 4%) and graft failure (5% and 2%),whereas PTLD have been reduced from 3% to 0,5%.
HSCT in pts with acquired SAA over the age of 40 years, continues to carry a significant risk of mortality , also in 2015, ranging from 30% in younger SIB transplants to over 50% in older pts. This study gives further support to current guidelines , suggesting first line therapy with ATG+CsA , in patients over the age of 40. Tailored protocols need to be devised to reduce transplant mortality in older SAA patients.
Peffault De Latour: Novartis: Consultancy, Honoraria, Research Funding; Alexion Pharmaceuticals, Inc.: Consultancy, Honoraria, Research Funding; Amgen: Research Funding; Pfizer: Consultancy, Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.